Kidney fibrosis, also known as renal fibrosis, is a pathological condition characterized by the excessive accumulation of extracellular matrix (ECM) proteins in the kidneys, leading to the formation of scar tissue. This fibrotic tissue replaces normal, functional renal tissue, impairing the kidney's ability to filter and excrete waste products and maintain fluid and electrolyte balance.
In the case of renal tubular epithelial cells, TGF-β can induce fibrosis by activating a complex signaling network involving various molecular pathways. When TGF-β binds to its receptor on renal tubular epithelial cells, it triggers the activation of downstream effectors, including Smad proteins. Smad proteins translocate into the nucleus, where they regulate the expression of genes involved in fibrosis, such as collagen, fibronectin, and connective tissue growth factor (CTGF). Additionally, TGF-β can modulate the epithelial-mesenchymal transition (EMT) process in renal tubular epithelial cells. EMT is a cellular program that converts epithelial cells into mesenchymal-like cells with enhanced migratory and invasive properties. During EMT, renal tubular epithelial cells lose their epithelial characteristics, including tight cell-cell junctions, and acquire a mesenchymal phenotype, which contributes to the development of fibrosis.
Creative Bioarray's TGF-β-induced Fibrosis on Kidney Cells offer a reliable and physiologically relevant model for studying various aspects of renal function and diseases. They have been extensively used in drug discovery and development to evaluate the efficacy and toxicity of candidate drugs, as well as to investigate the molecular mechanisms underlying renal diseases.
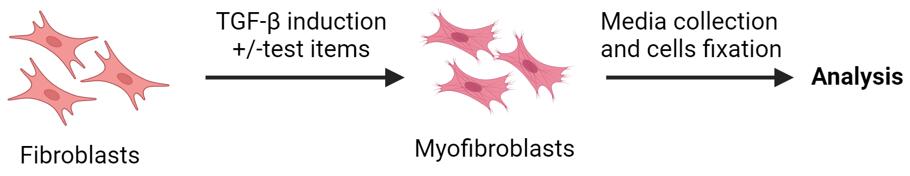 Fibroblast-to-myofibroblast transition (FMT)
Fibroblast-to-myofibroblast transition (FMT)
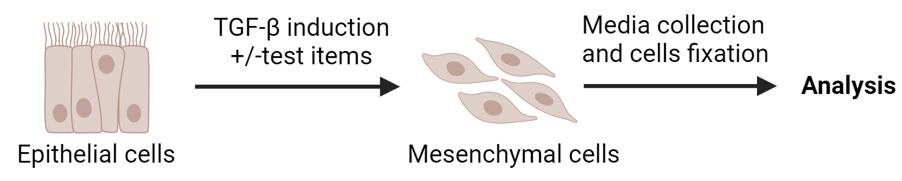 Epithelial-to-mesenchymal transition (EMT)
Epithelial-to-mesenchymal transition (EMT)
Study Examples:
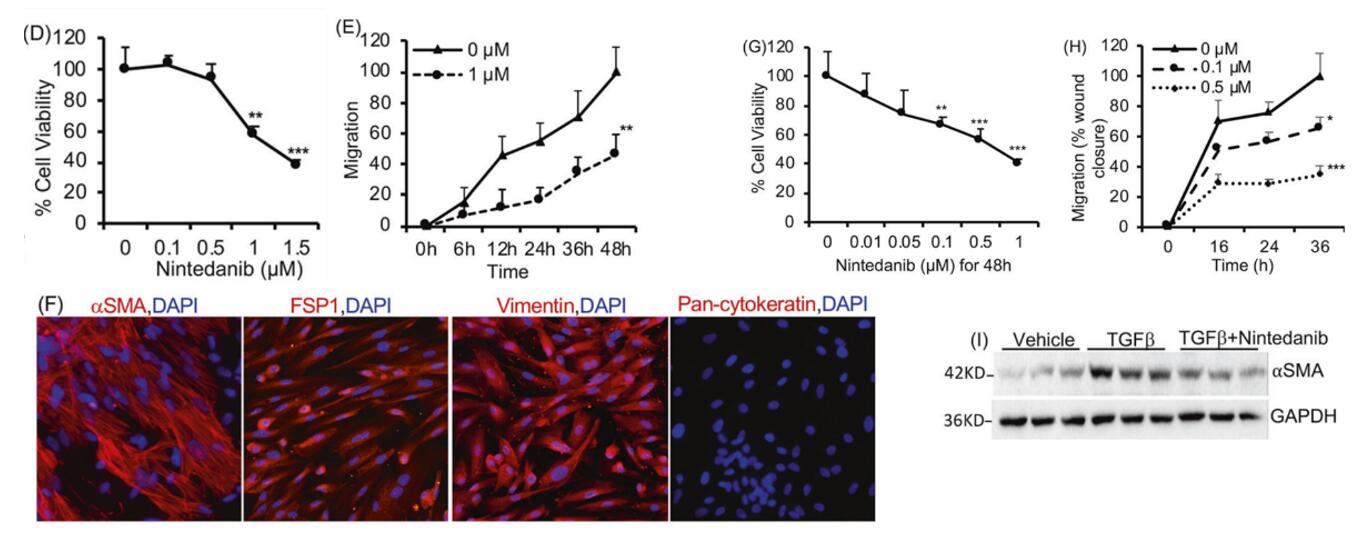 Figure 1. Effect of Nintedanib treatment on ADPKD renal cystic epithelial cells and myofibroblasts. D Human ADPKD renal myofibroblasts treated with nintedanib for 48 h. MTT assay and E migration (% wound closure in a scratch assay) in the presence of 0 or 1 µM nintedanib. F Human renal ADPDK myofibroblasts immunostained for αSMA, FSP1, vimentin, or pan-cytokeratin. G NRK-49F rat renal fibroblasts treated with nintedanib for 48 h. MTT assay. n = 7. H Migration of NRK-49F cells treated with nintedanib n = 4. I Immunoblot of NRK-49F cells incubated with TGFβ (2 ng/ml) and nintedanib (1.5 μM) for 48 h. [1]
Figure 1. Effect of Nintedanib treatment on ADPKD renal cystic epithelial cells and myofibroblasts. D Human ADPKD renal myofibroblasts treated with nintedanib for 48 h. MTT assay and E migration (% wound closure in a scratch assay) in the presence of 0 or 1 µM nintedanib. F Human renal ADPDK myofibroblasts immunostained for αSMA, FSP1, vimentin, or pan-cytokeratin. G NRK-49F rat renal fibroblasts treated with nintedanib for 48 h. MTT assay. n = 7. H Migration of NRK-49F cells treated with nintedanib n = 4. I Immunoblot of NRK-49F cells incubated with TGFβ (2 ng/ml) and nintedanib (1.5 μM) for 48 h. [1]
Reference:
1. Jamadar, Abeda et al. "The tyrosine-kinase inhibitor Nintedanib ameliorates autosomal-dominant polycystic kidney disease." Cell death & disease vol. 12,10 947. 14 Oct. 2021, doi:10.1038/s41419-021-04248-9
Online Inquiry